Coronary heart disease is the most common heart disease and the single most important cause of death.

Definition and overview
What is Coronary artery disease (CAD)?
Coronary artery disease (CAD) refers to the atherosclerotic narrowing of the epicardial coronary arteries. It may manifest insidiously as angina pectoris or as an acute coronary syndrome (ACS).
CAD can have the following clinical presentations:
- Asymptomatic
- Stable angina pectoris
- Unstable angina
- Myocardial infarction (MI)—either NSTEMI or STEMI Sudden cardiac death
What is The Major risk factors ?
- Diabetes mellitus (DM)—worst risk factor
- Hyperlipidemia—elevated low-density lipoprotein (LDL >160 mg/dL, HDL <40 mg/dL)
- Hypertension (HTN)—most common risk factor
- Cigarette smoking—There is a strong, dose-linked relationship between cigarette smoking and CAD.
- Age (Most important risk factor): Men ≥45 years old, women ≥55 years old
- Sex: Male > female, but post-menopausal female have same risk as male (estrogen protective).
- Family history of premature coronary artery disease (CAD) or myocardial infarction (MI) in first-degree relative: Men <55 years; women <65 years.
- A family history of premature CAD is established when there is definite myocardial infarction or sudden death before 55 years of age in a first-degree male relative, or before 65 years of age in a first-degree female relative.
Increased CRP, fibrinogen level, homocysetine level --> also increase risk of atherosclerosis.
How Atherosclerosis can lead to a heart attack?
Atherosclerotic narrowing resulting in coronary arterial obstruction is the cause of ischemic heart disease in almost 90% of the patients. Coronary stenosis >70% may be significant (i.e., it can produce angina).
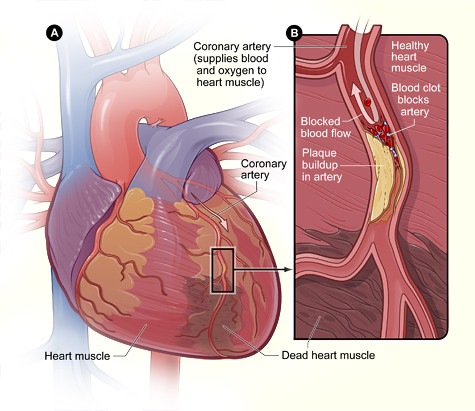 Heart With Muscle Damage and a Blocked Artery
Heart With Muscle Damage and a Blocked Artery
When does symptoms & signs of Atherosclerosis appear?
Atheroma remain clinically silent until:
- Atheroma becomes large enough to impair arterial perfusion (i.e. ischemia).
- Ulceration (discontinuation of the intimal layer over atheroma) leading to: Thrombus formations partial or complete obstruction or Embolization of the overlying thrombus or atheroma material.
- Weakening of the vessel may lead to aneurysm formation.
What is Difference between myocardial ischemia and myocardial infarction?
- Coronary ischemia is due to an imbalance between blood supply and oxygen demand, leading to inadequate perfusion.
- Acute myocardial infarction is defined as myocardial necrosis that occurs as a result of myocardial ischemia, and can be identified by the rise and fall of cardiac biomarkers in the blood (eg, cardiac-specific troponin) along with other supportive evidence (eg, characteristic electrocardiographic changes).
The main difference between angina and the MI is elevation of cardiac enzymes in the MI which is not seen usually with angina.
Stable Angina
Definition and overview
Stable angina pectoris is chest pain that occur when oxygen demand exceeds available blood supply. It's is due to transient myocardial ischemia without infarction (not necrosis).
It's usually due to fixed atherosclerotic lesions that narrow the major coronary arteries. but it may also occur in those with significant aortic stenosis, pulmonary hypertension, hypertrophic cardiomyopathy, coronary spasm, or volume overload.
Stable angina occurs when the myocardial oxygen demand is more than the supply; It takes place when the coronary artery is occluded >75%.
While it is not typically life threatening, it serves as a warning sign for potential heart attacks or strokes. By implementing treatment and adopting a healthy lifestyle, it is possible to manage angina and decrease the likelihood of these severe complications.
What is Difference between stable and unstable angina?
1) Typical stable anginal chest pain
- Substernal pressure sensation, usually described as heaviness, pressure, squeezing, tightness; rarely described as sharp or stabbing pain
- Pain is often gradual in onset, Lasts less than 10 to 15 minutes (usually 1 to 5 minutes)
- Brought on by factors that increase myocardial oxygen demand, such as exertion, stress, or drugs (i.e., cocaine or methamphetamines)
- Relieved with rest or nitroglycerin
2) Unstable angina is defined as angina pectoris or equivalent ischemic discomfort with at least one of three features:
- It occurs at rest usually lasting > 10 minutes
- It is severe and of new onset
- and/or it occurs with a crescendo pattern.
Note that ischemic pain does NOT change with breathing nor with body position. Also, patients with ischemic pain do not have chest wall tenderness. If any of these are present, the pain is less likely to be due to ischemia.
How to distinguish between stable and unstable angina clinically
- Stable angina chest pain it should last 3 to 10 minutes and be relieved by rest. If it lasts greater than 30 minutes, consider an acute coronary syndrome (ACS).
- Stable angina is usually relieved by rest or with sublingual nitroglycerin. Pts with symptoms of stable angina that fail to be relieved with three doses of nitroglycerin need to be evaluated for an ACS.
- Pts with stable angina present with symptoms that are evoked by the same level of activity (e.g., climbing two flights of stairs or walking more than 60 feet at a time). If the pt. provides a history of requiring less activity now to evoke the same symptoms, the pt is experiencing unstable angina, which is treated very differently.
What is Anginal equivalent ?
Patients may present without chest discomfort but with nonspecific or atypical symptoms such as dyspnea, diaphoresis, nausea, or indigestion that occur with exertion or stress. This called Anginal equivalent
Dyspnea on exertion may present as the only symptom. Atypical symptoms are more likely in women, the elderly, and diabetic patients.
Canadian Cardiovascular Society grading scale For angina
- Class I: Angina does not limit ordinary physical activity, occurring only with strenuous or prolonged exertion (7 to 8 metabolic equivalents [METs]).
- Class II: Angina causes slight limitation of ordinary activity. It occurs when walking rapidly, uphill, or >2 blocks; climbing >1 flight of stairs; or with emotional stress (5 to 6 METs).
- Class III: Angina causes marked limitation of ordinary physical activity. It occurs when walking 1 to 2 blocks or climbing one flight of stairs (3 to 4 METs).
- Class IV: Angina occurs with any physical activity and may occur at rest (1 to 2 METs).
How is CAD diagnosed?
What is the classic findings of stable angina on ECG?
Resting ECG: Usually normal in patients with stable angina (50% of patients), so normal ECG not exclude IHD.
The classic findings are ST-segment depression of at least 1 mm that is downward sloping during the ischemic episode and resolves after symptoms disappear.
If ST-segment or T-wave abnormalities are present during an episode of chest pain, then treat as unstable angina
Role of Stress ECG & Stress Echo in diagnosis of coronary artery disease
Exercise stress ECG is an ideal initial test if able to exercise and have a normal resting ECG (readily available and relatively inexpensive).
Stress testing is used in the following situations:
- To confirm diagnosis of angina
- To evaluate response to therapy in patients with documented CAD
- To identify patients with CAD who may have a high risk of acute coronary events
Stress ECG: Test involves recording ECG before, during, and after exercise on a treadmill or bicycle ergometer protocol.
A stress test is generally considered positive if the patient develops any of the following during exercise: ST-segment depression, chest pain, hypotension, or significant arrhythmias.
False positive test is seen, especially in patients with baseline ECG abnormalities such as left bundle branch block (LBBB), pre-existing ST-segment changes, or left ventricular hypertrophy (LVH), digoxin therapy.
Patients with a positive stress test result should undergo cardiac catheterization.
Contraindications to Exercise ECG:
- In pts. With acute MI within 2 days.
- Unstable angina until medically stabilized.
- Severe aortic stenosis.
- Uncontrolled hypertension
- Uncontrolled HF.
- Active pericarditis, myocarditis, endocarditis
Remember not to let any pt with a history of aortic stenosis perform a stress test, Sudden death may occur.
Stress Echo or Stress scintigraphy (perfusion scan): This is particularly helpful in patients who are unable to exercise or who have abnormal baseline ECG e.g. WPW, LBBB.
1) Method: Scintiscans of the myocardium are obtained at rest and during stress (exercise or pharmacological, e.g. dobutamine) after IV administration of a radioactive isotope that is taken up by viable perfused myocardium.
2) Diagnosis: Perfusion defect present during stress but not at rest indicates reversible myocardial ischaemia; a persistent defect suggests previous MI.
Again, patients with a positive test result should undergo cardiac catheterization.
Cardiac catheterization with coronary angiography
Cardiac Catheterization
Cardiac Catheterization: It's the Most accurate method of determining a specific cardiac diagnosis. Provides information on hemodynamics, intracardiac pressure measurements, cardiac output, oxygen saturation, etc.
Coronary angiography (see below) is almost always performed as well for visualization of coronary arteries.
Indications for cardiac catheterization
There are many indications for cardiac catheterization (generally performed when revascularization or other surgical intervention is being considered):
- After a positive stress test.
- Acute MI with intent of performing angiogram and PCI.
- In a patient with angina in any of the following situations: When noninvasive tests are nondiagnostic, angina that occurs despite medical therapy, angina that occurs soon after MI, and any angina that is a diagnostic dilemma.
- If a patient is severely symptomatic and urgent diagnosis and management are necessary.
- For evaluation of valvular disease, and to determine the need for surgical intervention.
Coronary angiography - The definitive test for CAD
Coronary angiography—definitive test for CAD: it's the most accurate method of identifying the presence and severity of CAD; the standard test for delineating coronary anatomy. This is the test of choice for patients with very high pre-test probability of CAD.
- It is indicated if noninvasive testing suggests a high-risk lesion or if patient fails to respond to appropriate medical management.
- The Main purpose is to identify patients with severe coronary disease to determine whether revascularization is needed.
- Contrast is injected into coronary vessels to visualize any stenotic lesions. This defines the location and extent of coronary disease.
- Revascularization with PCI involving a balloon and/or a stent can be performed at the same time as the diagnostic procedure.
- If CAD is severe (e.g., left main or three-vessel disease, or two-vessel disease with concurrent DM), refer patient for surgical revascularization (CABG).
Indication of Coronary angiography
- High risk stress ECG changes
- Convincing history with (–ve) stress ECG results (diagnosis uncertain).
- Symptoms uncontrolled by the use of 2 anti-anginal drugs.
- Post infarct angina or unstable angina.
- HF with angina.
- Patient <50 with angina or MI.
Treatment of Stable angina
Management decisions (general guidelines)
Lifestyle changes and optimal medical therapy must be emphasized to prevent progression of atherosclerosis and to control contributing risk factors.
- Lifestyle & Risk factor modification and aspirin are indicated in all patients.
- Treat acute symptoms with sublingual nitroglycerin Administer sublingual nitroglycerin every 3 to 5 minutes until symptoms resolve for up to three doses. If there is no relief, begin a workup and treatment to rule out ACS.
- If asymptomatic, give pharmacologic treatment to prevent further episodes of angina: Combine β-blockers, CCBs, and nitrates as tolerated, along with high-intensity statin therapy.
- Revascularization: Controversial for patients with stable CAD, as studies suggest no improvement in mortality and MI (when compared to medical therapy alone). Per guidelines, revascularization is indicated for stable angina refractory to medical therapy for symptom control.
Prevention of the progression of CAD, by Identification and control of risk factors:
- Smoking cessation (Smoking cessation cuts CAD risk in half by 1 year after quitting).
- HTN—vigorous BP control reduces the risk of CAD, especially in diabetic patients.
- Hyperlipidemia: Statins for hyperlipidemia target to keep the (LDL<100, HDL >35). The goal LDL is < 70 mg/dL in patients with known CAD.
- DM—type II diabetes is considered to be a cardiovascular heart diseaseequivalent, and strict glycemic control should be strongly emphasized.
- Obesity—weight loss modifies other risk factors (diabetes, HTN, and hyperlipidemia) and provides other health benefits.
- Exercise is critical: Exercise 30 minutes 4d/week; it minimizes emotional stress, promotes weight loss, and helps reduce other risk factors.
- Diet: Reduce intake of saturated fat (<7% total calories) and cholesterol (<200 mg/day).
Medical therapy for pt. With Stable angina
Standard of care for stable angina includes:
- Drugs that improve mortality: aspirin, high-intensity statins (or in some cases a PCSK9 inhibitor to lower LDL even further)
- Drugs that relieve angina: β-blockers, nitrates, calcium channel blockers, and ranolazine
1) Aspirin: Indicated in all patients with CAD Aspirin prevents thromboembolism in coronary circulation resulting in lower risk of MI (should be prescribed indefinitely for all patients with CAD). Clopidogrel is an equally effective alternative in patients intolerant of aspirin.
2) Lipid-lowering therapy - HMG-CoA reductase inhibitors (statins) lower LDL and reduce risk of CV death. PCSK9 inhibitors lower LDL even further than statins and have been found to reduce CV events in patients on statin therapy with LDL levels above 70
3) β-Blockers—block sympathetic stimulation of the heart Reduce HR, BP, and contractility, thereby decreasing cardiac work (i.e., β-blockers lower myocardial oxygen consumption)
4) Nitrates—cause coronary vasodilation and systemic venodilation.Relieve angina; reduce preload myocardial oxygen demand. May prevent angina when taken before exertion.
- Can be administered orally, sublingually, transdermally, intravenously, or in paste form. For chronic angina, oral or transdermal patches are used. For acute coronary syndromes, either sublingual, paste, or IV forms are used
5) Calcium channel blockers (CCBs): Cause coronary vasodilation and afterload reduction, reduce contractility. Add to antianginal therapy when β-blockers and nitrates are not fully effective.
The COURAGE trial showed essentially no difference in all-cause mortality and nonfatal MIs between patients with stable angina treated with maximal medical therapy alone versus medical therapy with PCI and bare metal stenting. Of note, most PCI is now done with drug-eluting stents which are superior to bare metal stents with regard to risk of stent thrombosis and recurrent MI.